Projects

This project is supported in part by grants from the Stavros Niarchos Foundation (SNF) Institute for Global Infectious Disease Research, the National Center for Advancing Translational Sciences, National Institutes of Health (NIH) Clinical and Translational Science Award (CTSA) #UL1-TR-000043 and the Agency for Healthcare Research and Quality (AHRQ) Grant 1P30-HS-021667.
Poster Presentation at SNF institute’s 2nd annual symposium at Rockefeller University
Chagas disease, caused by infection with protozoan parasite Trypanosoma cruzi, is an emerging parasitic infection in the United States. Also known as American trypanosomiasis, it affects an estimated 8 million people in Mexico, Central and South America, and approximately 240,000-350,000 people in the United States. The main route of infection is through insect vectors, most frequently triatomine bugs. Diagnosing Chagas disease can be complex and requires review of the patient history and history of potential exposure to insect vectors in endemic areas. Chagas disease treatment is available and very effective if prescribed during the acute phase, but the effectiveness diminishes the longer a person has been infected. In the USA, Chagas disease mostly affects migrant workers and immigrants from Mexico, Central America (El Salvador, Honduras) and South America (Bolivia, Venezuela, Brazil and Argentina), as well as travelers to these regions. Most Chagas disease cases in the USA are identified through blood donor screening for T cruzi-specific antibodies. These serologic testing can only identify patients with chronic Chagas infection. Local transmission and acute cases are far less often identified and reported.
This project is building a full-spectrum translational research team that engages community-based practicing primary care clinicians with laboratory scientists to examine a potential emerging Chagas disease epidemic in the USA.
For more information see: www.CDNetwork.org/Chagas

Funded by Administration on Aging Innovations in Nutrition Programs and Services, Department of Health and Human Services (DHHS), Administration for Community Living grant # HHS-2018-ACL-AOA-INNU00300, and the National Center for Advancing Translational Sciences, National Institutes of Health, through Rockefeller University, Grant # UL1 TR001866.
The Rockefeller University Center for Clinical and Translational Science (RU-CCTS), in partnership with the Carter Burden Network and Clinical Directors Network (CDN), tested a multifaceted intervention to lower blood pressure among seniors. CBN is a senior service organization promoting the well-being of seniors, with a significant clientele among minority and underserved populations. The program combined a dietary intervention delivered through communal meals at two senior centers, with educational, social, and behavioral interventions designed to improve self-efficacy around blood pressure self-management.High blood pressure poses significant health risks for seniors, increasing their risk for stroke, heart attack, heart failure, and kidney failure, all with an associated increase in mortality, morbidity, disability, cognitive and functional decline, and increasing healthcare costs. The health risks of high blood pressure are worsened by social disparities- racial and ethnic minorities and people of lower socioeconomic status are disproportionately affected. This project delivered a nutrition intervention along with educational activities intended to enhance seniors’ health knowledge and self-efficacy about blood pressure management. Ninety-four seniors receiving congregate meals at a neighborhood senior center participated in the project. They attended classes in nutrition and medication management and were provided with an automated BP monitor and trained to use it. Participants experienced a clinically meaningful decrease of 4.41 mmHg in systolic blood pressure at 1-month of DASH intervention, and of 6.9 mmHg at 6-month, demonstrating that collaborative implementation of this intervention can significantly lower systolic blood pressure among seniors.

The DASH project team and advisory committee members, 2019
Links:
- DASH Diet Intervention at Carter Burden Network Senior Centers
- Educational Videos on hypertension, cardiovascular disease and home blood pressure monitoring
- Poster for Translational Science, 2021: Primary Outcome
- Poster for Translational Science, 2019: Study Design
- Poster for Translational Science, 2022: Project Implementation
- ACL innovation awards
- Project Tools & Resources: ACL 2018 Grantees – Improving heart health through diet, education & self-efficacy
- A mechanistic study about the DASH diet, based on this community-engaged project : abstract & poster
- Publication (In Press): Implementing DASH-Aligned Congregate Meals and Self-Measured Blood Pressure in Two Senior Centers
Funded by RU-CCTS pilot grant & CTSA supplement & AHRQ Center of Excellence (P30) for Practice-Based-Research and Learning at Clinical Directors Network (CDN) Grant#1 P30-HS-021667

RU-CCTS leadership with clinicians and administrators from collaborating FQHCs
This study was conducted to learn about how Community Acquired Methicillin-resistant Staphylococcus Aureus (CA-MRSA) is identified and treated in Community Health Centers (CHCs) and determine the best methods for evaluating patients in the clinical setting and in the laboratory. CA-MRSA is an infection caused by the bacteria Staphylococcus Aureus that cannot be treated by common antibiotics. It is the most common cause of skin and soft tissue infections.The project established and tested the system and methods to identify, treat, culture and molecularly characterize CA-MRSA related infections across 6 collaborating community health centers in NYC and Texas, to learn better strategies to identify and manage patients who have been infected with CA-MRSA. It also laid the groundwork to conduct a larger comparative effectiveness research randomized controlled trial on treatment and outcomes (CAMP 2). The project aimed to create a strong, enduring bi-directional community engaged partnership among Community Health Centers (CHCs), Clinical Directors Network (CDN) and The Rockefeller University Center for Clinical and Translational Sciences (CCTS), and a robust infrastructure to enable the future conduct and dissemination of research addressing CA-MRSA skin and soft tissue infections (SSTIs).
Links:
 This project provided public health education and occupational safety training for barbershops and beauty salons to raise awareness about Community-Acquired Methicillin-Resistant Staphylococcus Aureus (CA-MRSA). The project developed and delivered a curriculum covering the infection risk of CA-MRSA, prevention of its transmission, and referrals to primary care for timely diagnosis and treatment.
This project provided public health education and occupational safety training for barbershops and beauty salons to raise awareness about Community-Acquired Methicillin-Resistant Staphylococcus Aureus (CA-MRSA). The project developed and delivered a curriculum covering the infection risk of CA-MRSA, prevention of its transmission, and referrals to primary care for timely diagnosis and treatment.
Reaching beyond the clinical setting to partner with community institutions is key in translating research into improved population health. Barbershops and beauty-parlors in many urban minority communities are often a source of health information for low-income and immigrant populations with limited English proficiency and limited health care access. In this initiative, they served as important hubs for disseminating public health information about MRSA. The project built upon the existing Community-Associated Methicillin-Resistant Staphylococcus Aureus Project (CAMP), a joint effort among Clinical Directors Network (CDN), The Rockefeller University Center for Clinical and Translational Science (RU-CCTS), and Community Health Centers (CHCs).
The project started when a community-based clinician on the CAMP steering committee highlighted the potential occupational risks to esthetic care professionals and their customers should MRSA lesions go unrecognized and proposed the opportunity to train barbers and other esthetic care workers to identify lesions. The clinician connected the CAMP team to a local community health advocate, a well-known and respected barber and small business leader in Harlem. As a businessman with 30 years of experience in the industry, he established a health advocacy and outreach organization and created a network of barbers/estheticians who are interested in learning more about health promotion.
A series of collaborative meetings followed between the barbershop health advocate, CDN, RU-CCTS research staff, and CHC clinicians to refine the study. The study team selected three neighborhoods in Manhattan, Brooklyn, and the Bronx , based on the presence of many barbershops and beauty salons in the area and the availability of a Community Health Center to act as a referral site. The study team worked with medical content experts, clinicians, the barbershop health advocate and several of his colleagues to develop accurate, culturally and linguistically-appropriate materials to engage and train the participating barbers. Education sessions, which typically lasted one hour, were delivered to the barbers and estheticians on-site, at a time coordinated with the shop owner that was most convenient for the staff. Informational videos, question and answer periods and role-playing exercises were utilized in the trainings to make the sessions engaging and interactive. The study found that estheticians were interested in receiving additional training on health education topics (such as serious chronic bacterial and viral infections) that they perceived were of direct relevance to their customers and staff. The educational intervention improved their knowledge of CA-MRSA and prevention measures. This increase in infection prevention knowledge was sustained for a period of at least two months after the sessions occurred.
Links:
Funded by: Patient Centered Outcomes Research Institute (PCORI, CONTRACT # CER-1402-10800) The Rockefeller University Center for Clinical and Translational Science (CCTS) Pilot Grants and Administrative Supplement (NIH-NCATS Grant # 8-UL1-TR000043) AHRQ Grant # P30 HS 021667
This project aimed to reduce the significant patient burden associated with recurrent Community-Acquired Methicillin-Resistant Staphylococcus aureus (CA-MRSA) ) and Community-Acquired Methicillin-Sensitive Staphylococcus aureus (CA-MSSA) skin and soft tissue infections (SSTIs). MRSA and MSSA are types of staph infections that are hard to treat and can spread to other people. They can lead to serious infections or even death. This project compared two ways to help patients keep MRSA and MSSA infections from coming back. All project participants were tested and treated by clinicians at a health center or emergency room. Additionally, all participants had a home visit from a team of two community health workers/promotoras specially trained to teach people about getting rid of staph. In the first way, the community health worker shared a pamphlet about living with MRSA. In the second way, the community health worker shared the pamphlet and gave instructions and materials for a five-day home hygiene plan for the patient and other willing household members. All patients received standard of care, including incision and drainage and/or oral antibiotics.
The project’s central hypothesis is that increases in MRSA knowledge, prevention self-efficacy, and decision-making autonomy will improve prevention behaviors, thereby reducing patient colonization and environmental contamination, which will lead to improved patient-centered, clinical, and public health outcomes. This project builds on a multi-stakeholder collaboration, including Clinical Directors Network (CDN), The Rockefeller University Center for Clinical and Translational Science (RU-CCTS), and Community Health Centers (CHCs) clinicians and staff.
Links:
- Publication: CAMP 2 study findings in Antibiotics, 2021
- Publication: Social Network Analysis of the CAMP1 and CAMP2 community academic partnership
- Final Research Report, PCORI
- Research Summary, PCORI
- Poster for Translational Science, 2018: Implementing and Evaluating an Evidence-Based Intervention from the ICU into Primary Care Using Promotoras to Reduce CA-MRSA Recurrence and Household Transmission

Funded by RU-CCTS pilot awards (NCATS/CTSA UL1 TR001866)

The Project team with members of RU, CDN and Carter Burden Network
The Rockefeller University Center for Clinical and Translational Science (RU-CCTS) and the Clinical Directors Network (CDN), formed a community-academic partnership with Carter Burden Network (CBN), a multi-site senior services organization serving East Harlem, NY. This partnership examined the use of a simple validated surrogate measure of overall health status and frailty in this population and aimed to build capacity, characterize the CBN senior population, and identify priorities and opportunities for community-engaged research. Many CBN seniors are racial/ethnic minorities, low-income, and suffer from multiple chronic conditions, depression and food insecurity. In addition, multiple biological, musculoskeletal, psychosocial and nutritional factors contribute to frailty. This project aimed to:
- Engage CBN seniors and stakeholders in priority-setting, joint protocol development, conduct, analysis and dissemination;
- Characterize the health status of the CBN seniors using validated measures;
- Establish data collection and data management infrastructure for research;
- Understand how attendance and utilization information routinely collected about health and senior activities can be used to create programs to improve senior health.
We assessed health and frailty measures in 218 high-risk seniors. Forty-one percent had a high school education or less, 67% had an income lower than the NY state federal income guideline, 83% were overweight or obese and one-third were moderately or severely frail. We also identified urgent health priorities including the need to control high blood pressure (see figure below).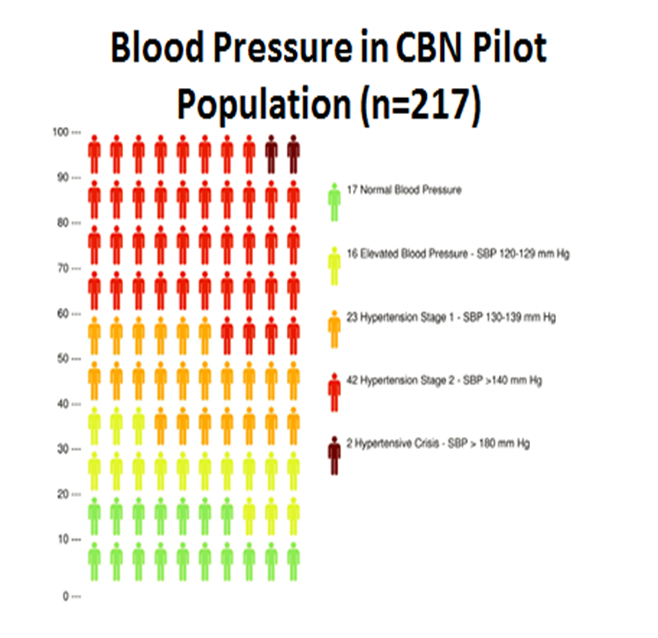
Links:

Funded by CTSA pilot award & PCORI

After the webcast on Dr. Emiliano’s research collaboration with practicing bariatric surgeons: Dr. Nemr, Dr. Emiliano, Dr. Kost and Dr. Tobin
We built a Full Spectrum Translational Research collaboration among Rockefeller University Clinical Scholar and endocrinologist, Dr. Ana Emiliano, CDN, and practicing bariatric surgeons and other clinicians at NYU/Lutheran Health Center in Brooklyn. Dr. Emiliano’s work focused on gut-brain communication underlying metabolic responses to bariatric surgery. This project sought to correlate patient pre- and post-surgery metabolic data extracted from EHRs with experimental mouse bariatric surgery models. With Rockefeller CTSA pilot project funding and leadership from the CDN/N2-PBRN (Dr. Tobin), this collaboration blossomed over 6 years into becoming a part of a national PCORI-funded network ’Big Data’ study involving clinical data research networks (CDRNs), patient powered research networks (PPRNs), and many CTSA Hubs.
Links:

 The purpose of this study was to determine if disproportionate health burdens are experienced by low income, minority pregnant adolescents and their offspring up to the age of 24 months. Investigating adolescent and young adult nutritional status, pregnancy rates and birth outcomes require rigorous “Big Data” analysis. We established a multisite de-identified database aggregating clinical, behavioral, health services, and social determinants measures from populations attending NYC Community Health Centers to test the use of these data to predict nutritional status and pregnancy outcomes for adolescent females and their infants.Investigators convened a group of clinical leaders from multiple community health centers serving low-income and minority communities in order to develop relevant clinical, behavioral, health services, and social behavioral measures to include in the multisite de-identified database.
The purpose of this study was to determine if disproportionate health burdens are experienced by low income, minority pregnant adolescents and their offspring up to the age of 24 months. Investigating adolescent and young adult nutritional status, pregnancy rates and birth outcomes require rigorous “Big Data” analysis. We established a multisite de-identified database aggregating clinical, behavioral, health services, and social determinants measures from populations attending NYC Community Health Centers to test the use of these data to predict nutritional status and pregnancy outcomes for adolescent females and their infants.Investigators convened a group of clinical leaders from multiple community health centers serving low-income and minority communities in order to develop relevant clinical, behavioral, health services, and social behavioral measures to include in the multisite de-identified database.
The project’s community-academic partnership contributed to the creation of a multi-site de-identified Electronic Health Records (EHR) database that uses available measures from routine clinical care as a “rapid assay” to explore associations and identify targets for future interventions to address adolescent nutritional and pregnancy outcomes. This partnership has engaged community clinicians, investigators and funders in study design and analysis. Preliminary findings have found associations between maternal BMI group and birth outcomes. The study is being replicated using data from NYC Academic Health Centers. This rich database has proved useful for hypothesis generation and testing for other questions related to obesity and adolescent health.
Links:
Poster for Translational Science, 2021: Obesity-Related Renal Damage in Adolescent Women

Funded by Funded by NCATS, NIH, Robertson Therapeutic Development Fund, Bernard and Irene Schwartz Foundation, the Rheumatology Research Foundation and the Simons Foundation.Dr. Dana Orange studied a group of patients with rheumatoid arthritis to learn what happens in the immune system before flares. Rheumatoid arthritis flares are hard to predict and involve worsening joint symptoms such as pain, swelling and stiffness. For this study, patients recorded their symptoms and collected their own blood by finger stick at home and mailed blood samples and symptom questionnaires to the laboratory for analysis. This new collection method enabled researchers at Rockefeller University to study blood samples just prior to flares and to identify what changes in the blood right before symptoms develop.
Dr. Orange discovered a new type of cell called PRIME cells (PRe-Inflammatory MEsenchymal). PRIME cells are present in the blood of rheumatoid arthritis patents. The appearance of PRIME cells in the blood predicts a flare a week or two before symptoms start. Discovering PRIME cells has opened a new area of study in understanding how arthritis develops. Finding a predictor of flare could lead to new approaches to detecting, treating, or even preventing flares. Now we will work to understand what activates B cells and then PRIME cells prior to rheumatoid arthritis flares. Researchers will also continue to study flares to see if different immune events occur in different people.
Links:
Publication: RNA Identification of PRIME Cells Predicting Rheumatoid Arthritis Flares

This study was funded by grant # UL1 TR001866 from the National Center for Advancing Translational Sciences (NCATS), National Institutes of Health (NIH), and the Patient Centered Outcomes Research Institute (PCORI) PCORnet grant to the NYC-CDRN grant # CDRN-106-03961.
People with prosopagnosia (face blindness) have great difficulty perceiving, recognizing, or memorizing faces, even those of very familiar people. Living with prosopagnosia can negatively impact the affected person’s quality of life. Before conducting this study, little was known about the epidemiology of prosopagnosia. We did not have good ways of tracking the characteristics of the population such as gender, age, race, and/or which other diagnoses or conditions people with prosopagnosia also have.
 In this project, we used information from a collection of more than 7 million de-identified electronic health records to study the characteristics of people with prosopagnosia as compared to controls and find out how common the diagnosis is. We discovered that prosopagnosia does not get diagnosed as often as we thought. While, it has been reported that prosopagnosia may affect up to 1 in 33 individuals, we identified only 12 in 100,000 individuals had been diagnosed with the condition across NYC academic and community health centers. We further discovered that individuals who were diagnosed with prosopagnosia were more likely to also be diagnosed with other conditions, such as depression, anxiety, personality disorder, and/or epilepsy. Moreover, we found that the likelihood of carrying the diagnosis code for prosopagnosia increased with the number of comorbid condition diagnoses.
In this project, we used information from a collection of more than 7 million de-identified electronic health records to study the characteristics of people with prosopagnosia as compared to controls and find out how common the diagnosis is. We discovered that prosopagnosia does not get diagnosed as often as we thought. While, it has been reported that prosopagnosia may affect up to 1 in 33 individuals, we identified only 12 in 100,000 individuals had been diagnosed with the condition across NYC academic and community health centers. We further discovered that individuals who were diagnosed with prosopagnosia were more likely to also be diagnosed with other conditions, such as depression, anxiety, personality disorder, and/or epilepsy. Moreover, we found that the likelihood of carrying the diagnosis code for prosopagnosia increased with the number of comorbid condition diagnoses.
These results are important for people living with prosopagnosia, their caregivers, and family members, as well as health care providers. Findings from this study are important as they will raise awareness on prosopagnosia and inform the medical community about the other conditions that are often associated with it. Results from this study will help guide further investigations of the relationships between prosopagnosia and other conditions, potentially leading to better care and diagnosis.
Links:
(2018-ongoing)

Hidradenitis suppurativa (HS) is a chronic skin disease which disproportionately affects women, and Black and Hispanic patients. Until recently, there were no approved treatments for this painful and disfiguring disorder.
 In 2018, researchers in Dr. Krueger’s Laboratory of Investigative Dermatology turned their attention to studying the basic biology of HS. Clinical Scholar Dr. John Frew and Dr. Krueger partnered with Dr. Michelle Lowes of the Hidradenitis Foundation to reach out to the HS population. We wanted to understand patient’s priorities, concerns and interests. To do this, we held a Full Spectrum Town Hall meeting called Shedding Light on HS (also streamed on the internet) – combining presentations that address the basic biology of HS, a description of the clinical disease, an explanation of Dr. Krueger’s translational approach to understanding skin diseases, and a panel of patients sharing their experiences with HS, all in language accessible to the general public. After our 2018 Town Hall meeting, we then conducted a Community Engagement Studio, meeting with 11 patients-as-experts to refine the design of the first HS research protocols to be conducted at the CCTS. Dr. Frew incorporated patients’ suggestions into the design of his first HS studies.
In 2018, researchers in Dr. Krueger’s Laboratory of Investigative Dermatology turned their attention to studying the basic biology of HS. Clinical Scholar Dr. John Frew and Dr. Krueger partnered with Dr. Michelle Lowes of the Hidradenitis Foundation to reach out to the HS population. We wanted to understand patient’s priorities, concerns and interests. To do this, we held a Full Spectrum Town Hall meeting called Shedding Light on HS (also streamed on the internet) – combining presentations that address the basic biology of HS, a description of the clinical disease, an explanation of Dr. Krueger’s translational approach to understanding skin diseases, and a panel of patients sharing their experiences with HS, all in language accessible to the general public. After our 2018 Town Hall meeting, we then conducted a Community Engagement Studio, meeting with 11 patients-as-experts to refine the design of the first HS research protocols to be conducted at the CCTS. Dr. Frew incorporated patients’ suggestions into the design of his first HS studies.
In the two years that followed, Drs. Frew and Krueger conducted research studies and made numerous major discoveries about the biology of HS that are informing the development of new treatments. Dr. Frew published over 50 papers addressing scientific and clinical aspects of HS, a major contribution to this previously under-studied disease. One of the therapies tested showed great promise for dramatically improving treatment options for patients with HS.
To continue our engagement with the HS community and return the results from the recent clinical studies directly to the community, we conducted a second Full Spectrum Research Town Hall meeting, Shining Light on HS. A Dr. John Frew returned results from clinical trials conducted at Rockefeller University and discussed the implications of the research findings for future diagnosis and treatment of HS. Dr. Yael Renert-Yuval, also in Dr. Krueger’s group, presented on a new study on HS that she recently developed. Over 150 individuals, including patients, clinicians, researchers, and members of the pharmaceutical industry, attended the webinar.
Our experience with HS exemplifies one very important aspect of translational research, that is the cycling between “Bedside to Bench” –the patient experience, and clinical information and samples (bedside) inform the basic science (bench) – alternating with Bench (scientific discovery) to Bedside (implemented as new therapies tested/demonstrated). This cycling illustrates why an ongoing and bidirectional partnership between scientist, clinicians and patients, is critical to advancing research for the benefit of patients.
Links:

Funded by RU-CCTS pilot grant.
Autoimmune polyglandular syndrome type 1 (APS1) is an ultra-rare disorder, with fewer than 100 documented cases in North America. It can cause complex and potentially life-threatening symptoms. The median life expectancy among people with APS1 is only 33 years of age, due in large part to diagnostic delays and lack of timely treatment of symptoms.
A recent study of 35 patients with APS1 suggested that the classification criteria might be expanded to include three additional criteria (specifically urticaria, intestinal dysfunction and ectodermal dysplasia). These expanded criteria could facilitate diagnosis prior to development of life-threatening complications. However, the specificity of these expanded criteria is not known, and they have therefore not been adopted into clinical practice.
To address this problem, a community-academic partnership of investigators at the Rockefeller University and The APS Type 1 Foundation Inc., comprised of families affected by APS1, plan to compute the: i) frequency of patients meeting standard, or expanded diagnostic criteria for the APS1 phenotype data from the New York City Clinical Data Research Network (INSIGHT-CRN) database. This work will identify the optimal clinical criteria for earlier diagnosis, prior to development of life-threatening manifestations. This work also provides a framework for leveraging health record data to compute phenotype frequency for case-finding in other rare diseases.

The Fanconi anemia patient registry is a patient-facing, longitudinal study to elucidate the biology underlying this genetic disease. Fanconi Anemia is caused by a genetic mutation in the basic DNA repair mechanisms, a flaw that leads to many uncorrected mutations in the blueprints governing many basic functions of the body.The Registry began as families of young patients with Fanconi anemia organized to help researchers study the disease and improve treatment. The Registry host a database where people who may have Fanconi Anemia, and their close family members can share information about the disorder. The researchers collect longitudinal (over time) information about the medical history, genetics, clinical course, blood test results, treatment, complications and social issues of Fanconi Anemia. Tissue samples are also collected in a repository in order to study the genotype of the study subjects, for geneotype/phenotype correlation and to understand why the disease develops. The project studies the nature, diagnosis and treatment of individuals affected with this inherited disorder that leads to bone marrow failure (aplastic anemia).
The study of Fanconi anemia has improved our understanding of normal bone marrow function and the development of cancer.


This project is supported in part by a Collaborative Innovation Award from the National Center for Accelerating Translational Science #U01TR003206 to the Rockefeller University, and Clinical Translational Science Awards UL1TR001866 (Rockefeller University), UL1TR002553 (Duke University), UL1TR003098 (Johns Hopkins University), UL1TR002001 (University of Rochester), UL1TR002243 (Vanderbilt University), and UL1TR001420 (Wake Forest University Health Sciences)
To develop research projects that are embedded in community needs, it is essential to learn about the experience of research participants and take their perspective into account. The CRSO has led a multi-institutional set of projects to develop and disseminate a Research Participant Perception Survey (RPPS) to gather participant perspective. The RPPS surveys are validated, which means that they have passed tests of reliability and reproducibility in collecting the information. The RPPS offered insights into research participants’ experiences that had not previously been collected at scale or using a valid tool. We fielded the survey to thousands of participants and analyzed their responses. The surveys give researchers the tools to empirically test to find the best approaches to recruitment, consent, study conduct, compensation, return of results, and more from the perspective of the participants. The surveys can be used over time to test different approaches to enhance informed consent, outreach, recruitment, return of results and other aspects of research.
For more information see: https://www.rucares.org/clinicalresearch/dept/crso/strategies
To build on our findings from the RPPS, we recently launched another multi-institutional project called Empowering the Participant Voice. The project is designed to overcome barriers to using the RPPS that institutions have faced previously when thinking about collecting feedback. Through collaboration across six Clinical and Translational Science Award sites (CTSAs), the team will engage institutional, community, and patient stakeholders as they develop tools, standards, focus on how to best reach different populations and how to make results valuable to different audiences.
* 
This is the translational science spectrum. The highlighted stages apply to the projects above.


