Genetic mutation helps explain why, in rare cases, flu can kill
Nobody likes getting the flu, but for some people, fluids and rest aren’t enough. A small number of children who catch the influenza virus fall so ill they end up in the hospital — perhaps needing ventilators to breathe — even while their family and friends recover easily. New research by Rockefeller University scientists, published March 26 in Science, helps explain why: a rare genetic mutation.
The researchers scrutinized blood and tissue samples from a young girl who, at the age of two-and-a-half, developed acute respiratory distress syndrome after catching the flu, and ended up fighting for her life in the hospital. Years after her ordeal, which she survived, scientists led by Jean-Laurent Casanova discovered that it could be explained by a rare mutation she carries that prevented her from producing a protein, interferon, that helps fight off the virus.
“This is the first example of a common, isolated and life-threatening infection of childhood that is shown to be also a genetic disease,” says Casanova. The good news from these results, however, is that clinicians have a new treatment option for children who mysteriously develop severe cases of the flu. “This finding suggests that one could treat severe flu of childhood with interferon, which is commercially available,” says Casanova, who is professor and head of the St. Giles Laboratory of Human Genetics of Infectious Disease at Rockefeller, as well as a Howard Hughes Medical Institute investigator.
The fact that a child’s genes could affect the severity of her illness wasn’t a surprise to the members of Casanova’s lab, who have been studying this phenomenon for decades. For instance, they have discovered genetic differences that help explain why the herpes simplex virus — which causes innocuous cold sores in most people — can, in rare cases, lead to potentially fatal infections that spread to the brain.
Turning their attention to influenza, Michael J. Ciancanelli, a research associate and senior member of Casanova’s lab, and his colleagues sequenced all genes in the genomes of the young girl who survived her dangerous bout of the flu and her parents, looking for mutations that might explain her vulnerability. Knowing how rare her reaction to the flu was, they narrowed their search to mutations that were unique to her, then focused only on those that affected the immune system.
What emerged from their work was the finding that the girl had inherited two differently mutated copies of the gene IRF7, which encodes a protein that amplifies the production of interferon, a critical part of the body’s response to viral infections. “No other mutations could have explained her reaction to the influenza virus,” says Ciancanelli. “Each mutation is very uncommon and thus the likelihood of carrying two damaged copies of the gene is extremely rare.”
Indeed, when they infected a sample of her blood cells that normally produce interferon —plasmacytoid dendritic cells — the researchers measured no interferon. In contrast, blood cells from her parents, who each carried only one mutated version of the gene, produced healthy amounts of interferon when exposed to influenza. “That really was definitive proof that a single, non-mutated copy of this gene is enough to allow people to mount a response to the virus,” says Ciancanelli.
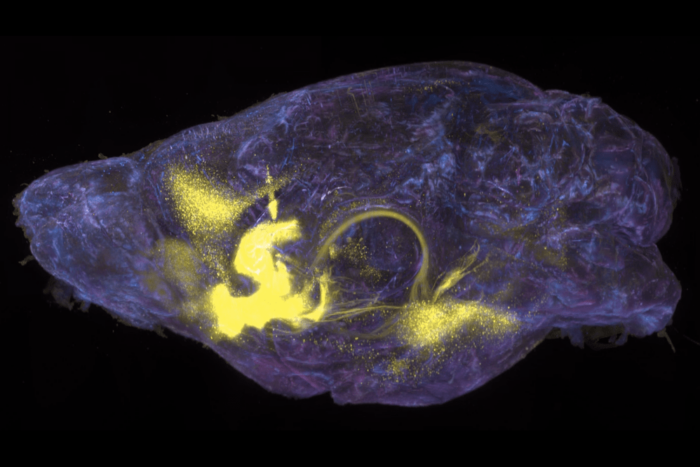
The researchers also employed a cutting-edge technology developed by their collaborators at Columbia University to reprogram the child’s skin cells into early progenitor cells, then differentiate those into lung cells, the front lines of influenza infections. Not surprisingly, the virus replicated more in the patient’s cells than in the same cells from healthy people.
Although the patient remains susceptible to severe reactions to new influenza viruses, annual vaccination against seasonal flu has, so far, prevented the occurrence of severe symptoms, indiciating that IRF7 is not needed for adaptive immunity to secondary infection by a flu virus.
Moreover, she hasn’t fallen nearly as ill from other viruses, suggesting her lack of IRF7-dependent interferon production may not leave her vulnerable to viruses overall — a situation the researchers say they have also noted with other mutations that underlie infectious disease.
 |
Science online: March 26, 2015 Life-threatening influenza and impaired interferon amplification in human IRF7 deficiency Michael J. Ciancanelli, Sarah X. L. Huang, Priya Luthra, Hannah Garner, Yuval Itan, Stefano Volpi, Fabien G. Lafaille, Céline Trouillet, Mirco Schmolke, Randy A. Albrecht, Elisabeth Israelsson, Hye Kyung Lim, Melina Casadio, Tamar Hermesh, Lazaro Lorenzo, Lawrence W. Leung, Vincent Pedergnana, Bertrand Boisson, Satoshi Okada, Capucine Picard, Benedicte Ringuier, Françoise Troussier, Damien Chaussabel, Laurent Abel, Isabelle Pellier, Luigi D. Notarangelo, Adolfo García-Sastre, Christopher F. Basler, Frédéric Geissmann, Shen-Ying Zhang, Hans-Willem Snoeck, and Jean-Laurent Casanova |