Cancer stem cells identified, offering new drug targets
Like carpet bombing, traditional chemotherapy is not very discriminating. Both can cause disastrous collateral damage and still fail to take out the real enemy. New research offers the potential for a surgical strike against cancer that would target only its root cause — cancer stem cells. Elaine Fuchs, head of Rockefeller University’s Laboratory of Mammalian Cell Biology and Development, and her postdoctoral fellow and first author, Markus Schober, have identified stem cells of squamous cell skin carcinoma, the second most common cancer in the world, and their molecular signature. The researchers find differences between cancer stem cells and healthy skin stem cells, which provide an invaluable diagnostic marker and suggests the possibility to specifically target the root of cancer while leaving normal cells unaffected.

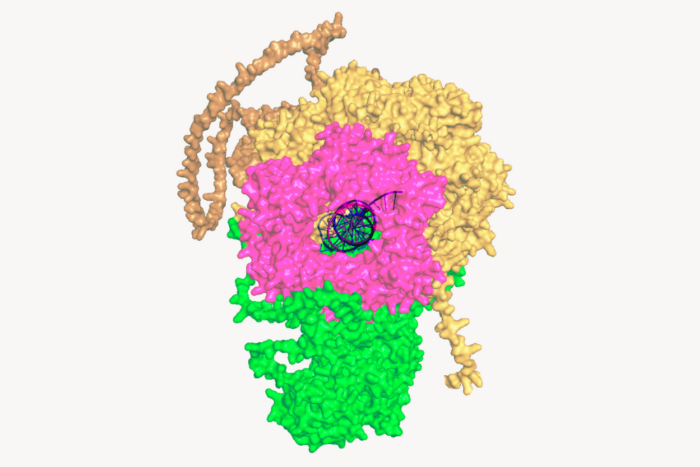
Managing aggression. Researchers in Elaine Fuchs’ lab have identified stem cells of squamous cell skin carcinoma, the second most common cancer in the world, and their molecular signature. Squamous cell carcinoma contains undifferentiated cells (red) at the tumor stroma interface, which sustain long term tumor growth and differentiate (green) into keratinized pearls at the tumor center.
“We’ve discovered that within these skin cancers, there exist cells — so-called cancer stem cells — that can continually churn out tumor tissue in a fashion analogous to our normal skin stem cells, which continually rejuvenate the epidermis and hairs on our body and repair our wounds,” says Fuchs.
The research, published this week in Proceedings of the National Academy of Sciences, focused on four groups of mice which carried mutations in genes which are commonly deregulated in human cancers. The first had defects in a gene that made the mice prone to cancer; the second had mutations in a gene that made them more resistant; the third had mutations in both genes, which made them susceptible to cancer at the same rate as normal mice, which composed the fourth group. When the four groups of mice were exposed to the chemical mutagen DMBA, the mice developed malignant squamous skin cell carcinomas that varied in degrees of aggression.
To identify the mechanisms by which mutations in these genes either promote or restrict tumor growth, the researchers started to fractionate the complex mix of cancer cells to identify the cancer stem cells, which can seed new tumors when injected into tumor free mice. Finally, they compared the genetic profile of these tumor-generating cancer stem cells to that of normal skin stem cells, providing investigators with reliable markers to tell the two apart.
Interestingly, the aggressive tumors contained more proliferative cancer stem cells than less aggressive tumors, indicating that when these skin cancers lose their ability to respond to growth inhibitory TGF-β signals from the tumor stroma, they can become very aggressive. In addition, the stem cells of all the skin cancers expressed a number of genes that readily distinguished them from normal stem cells.
In the process, the researchers also manipulated the activity of important molecular signaling pathways in the tumor cells to look for differences that cause more or less aggressive and numerous carcinomas. Specifically, they found that carcinomas with an active TGF-β pathway were fewer and less aggressive; those with an active FAK/integrin pathway were more malignant.
“By taking advantage of this new information, it may be possible in the future to design drugs to reduce the expansion and survival as well as the aggressiveness of the cancer stem cells, without harming the normal stem cells of the tissue” says Fuchs, who is Rebecca C. Lancefield Professor at Rockefeller and an investigator with the Howard Hughes Medical Institute.