Clinical study to probe genetic link to Salmonella diseases
Depending on your genes, Salmonella can mean a lot more than food poisoning. In a new clinical study, researchers at The Rockefeller University Hospital are narrowing in on the genetic link that predisposes a person to a set of complications known as severe nontyphoidal salmonellosis (SNTS). The study will analyze medical records and blood samples of SNTS-diagnosed children and may clarify the role of genetics in the immune system’s various responses to Salmonella infection and lead to more efficient treatments for the disease.
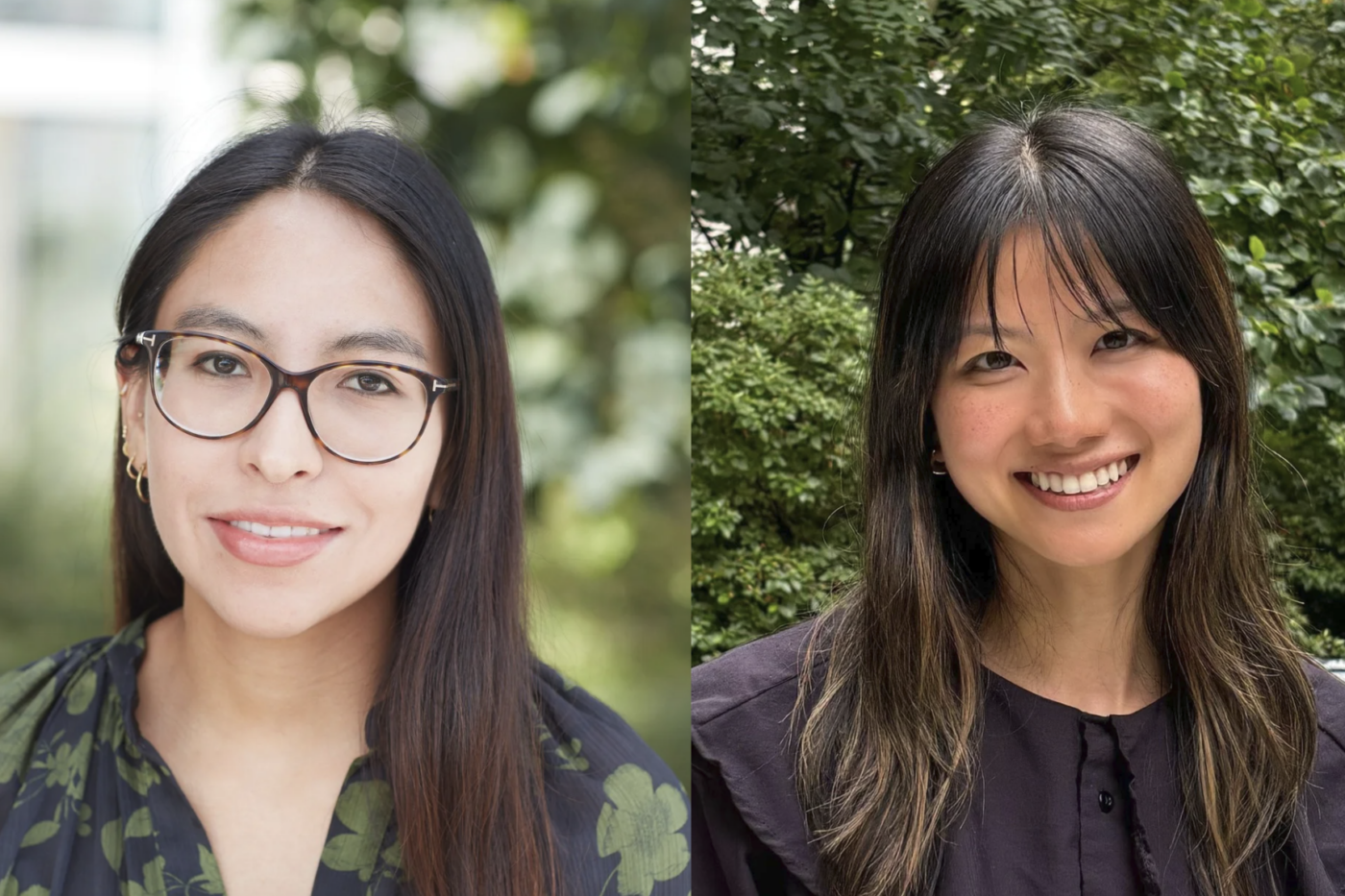
Certain strains of Salmonella are well known for their virulence. Salmonella typhi, for example, causes typhoid fever, which results in more than half a million deaths each year in the developing nations where it is endemic. But S. typhi is a plain-dealing villain. “The symptoms associated with typhoidal Salmonella are the same regardless of the host’s immunological profile,” says Carolina Prando, a postdoctoral fellow in Jean-Laurent Casanova’s Laboratory of Human Genetics of Infectious Diseases and the co-principal investigator of the study with Research Associate Stephanie Boisson-Dupuis. Nontyphoidal strains, on the other hand, are the con artist of the Salmonella family: They are a frequent culprit behind food poisoning in healthy children, but in children with impaired immunity, can also wreak havoc in any number of organ systems, producing liver or spleen abscesses, bone infections, meningitis or other disease states. “These symptoms are decidedly non-gastroenterological; they are not symptoms normally produced by nontyphoidal Salmonella in healthy children,” says Prando.
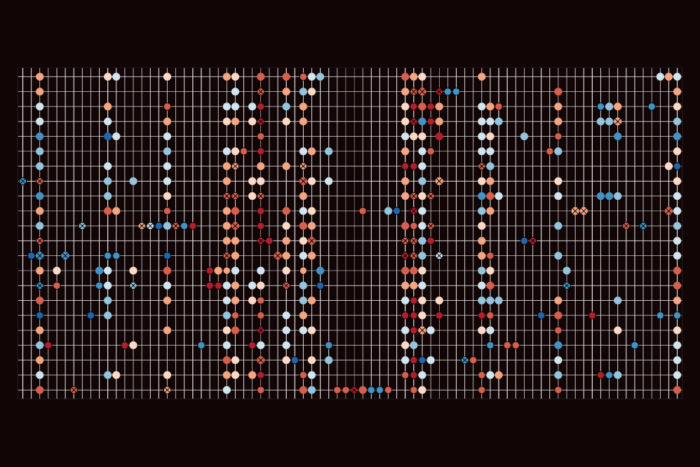
Casanova’s laboratory, which moved from the Necker Medical School in Paris to Rockefeller University last year, has for over a decade been one of the world’s major centers of research on human genetic causes of mycobacterial disease. His group has identified six genes whose mutations predispose a person to mycobacterial infection through the disturbance of key signaling pathways of the immune system. The new study aims to find similar disturbances connected to SNTS.
The investigators’ past work has shown that among patients with mutations in the IFN-γ-dependent part of a circuit known as IL-12/23-IFN-γ, there is a five percent incidence of SNTS associated with mycobacterial disease, while more than 50 percent of patients with a mutation in another part of the circuit are predisposed toward development of both mycobacterial and SNTS infections. However, even these known genetic defects do not explain all the cases. A large fraction of children with SNTS — especially children with isolated SNTS without mycobacterial disease — still lack a genetic explanation.
The new study focuses on the pathway of the signaling molecule known as IL-23. Working with data supplied by pediatricians whose patients had presented with SNTS affecting bones, lymph nodes, the central nervous system and other areas, the investigators currently have 40 subjects for the study and aim to gather data on at least 60 more. By mapping out genes involved in the IL-23-dependent pathway, Prando and Boisson-Dupuis hope to pinpoint the genetic cause behind the unexplained cases of SNTS, and to more definitively distinguish the pathways that lead to mycobacterial disease from those that lead to SNTS. “If we are correct, then a known genetic mutation or history of infection in one family member can suggest the right diagnostic testing for other family members,” says Boisson-Dupuis. “Therapeutically, new approaches based on replacing what’s missing in the immune system may be developed.”