New faculty member seeks secrets of intestinal immunity
Daniel Mucida, a scientist who studies the mechanisms of intestinal immunity, has been named assistant professor and will join Rockefeller University as head of the Laboratory of Mucosal Immunology in September. Mucida’s appointment was the result of the university’s fall 2009 open faculty search.
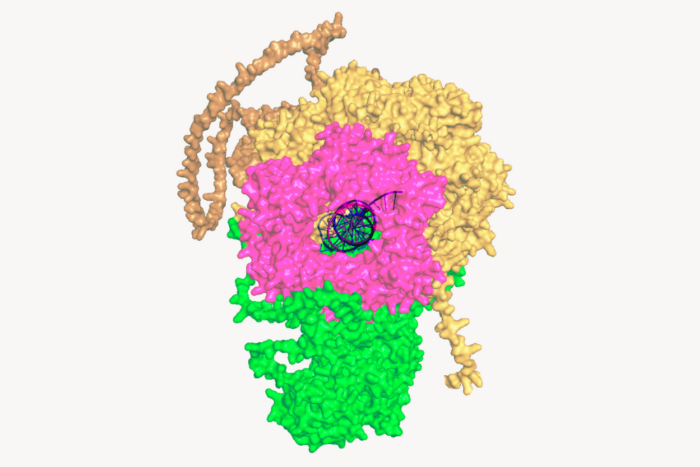
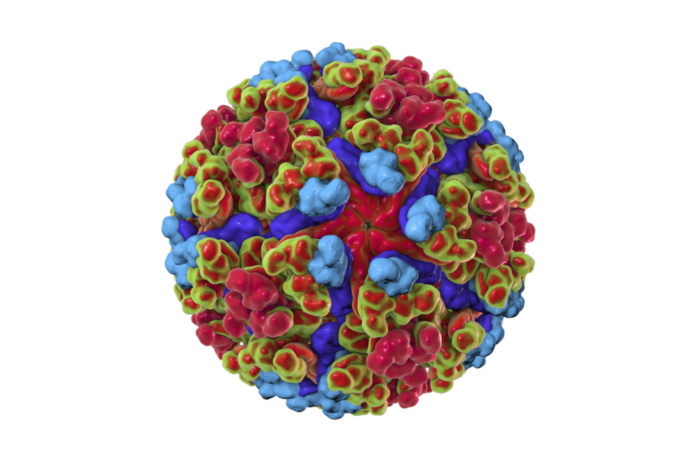
Mucida is interested in understanding how the immune system is able to respond to pathogens without jeopardizing its tolerance to innocuous substances, a critical balance that allows us to fend off infectious disease without inflicting damage on our own tissues. He studies this process in the intestines, where the body must cope with a constant stream of foreign antigens from food as well as a flourishing ecosystem of bacteria, viruses and parasites.
“The intestine is one of the best places to study immunology,” says Mucida. “There are more lymphocytes in the intestines than there are everywhere else in the body combined, and they must not only recognize and clear harmful pathogens, but also maintain tolerance toward an enormous variety of different antigens that they are exposed to every day.”
A native of Brazil, Mucida attended the Federal University of Minas Gerais in the Brazilian city of Belo Horizonte, graduating in 2000. It was there that his broad childhood interest in physics, math, genetics and marine biology evolved into a fascination with the workings of the immune system. For his Ph.D. work he focused on tolerance in mucosal tissues — not just those of the mouth and digestive tract, but also of the nose and respiratory system. Working primarily in mice, he made discoveries about how specific immune system cells — lymphocytes and T cells — contribute to “oral tolerance,” our ability to avoid reacting to what we ingest. He received his Ph.D. jointly from the University of São Paulo in Brazil and New York University in 2005.
As a postdoc he has spent time at both the University of São Paulo and the La Jolla Institute for Allergy and Immunology near San Diego, where he has been since 2006. His work in La Jolla has focused on the role of diet and bacteria in intestinal immunity. In 2007 he showed that a vitamin A metabolite, retinoic acid, produced by intestinal dendritic cells, is able to modulate the development of inflammatory and regulatory cells. His recent studies in germ-free mice, which do not develop a mature immune system, have shown how interactions between bacteria and CD4 helper T cells are crucial to modulating the cells’ inflammatory activity.
“We are very fortunate to have recruited Daniel to Rockefeller,” says Paul Nurse, the university’s president. “His work on immunity and the relationship between intestinal bacteria and inflammation is very innovative and has the potential to teach us much about how we might someday harness the power of the immune system to fight infectious disease and prevent autoimmune conditions such as asthma.”
“Our work isn’t just about intestinal infections, food poisoning and food allergy, but also pertains to infections that originate in other systems,” Mucida says. “Many viruses, for instance, use the gut to replicate and spread regardless of their point of entry. In addition, antibodies which form in response to foreign bodies in the gut can help the body’s immune system correctly identify threats elsewhere in the body.”