Rockefeller Researchers Clone Gene for Obesity
Fifty years after the discovery at Rockefeller University that genes are made of DNA, Dr. Jeffrey M. Friedman of the Howard Hughes Medical Institute at Rockefeller University and a team of Rockefeller researchers has cloned the first recessive obesity gene in mice and its human homologue, opening a new era for the understanding and, potentially, the treatment of obesity.
Torsten Wiesel, the Nobel Prize-winning neurobiologist who is president of The Rockefeller University, said: “This finding is a major breakthrough because it gives researchers a powerful new tool for understanding the mechanisms that regulate body weight. We now anticipate many additional discoveries in the field and eventually even the possibility of devising new drug therapies to treat obesity, a serious disease that predisposes people to such potentially life-threatening conditions as diabetes, heart disease and high blood pressure.”
Purnell W. Choppin, M.D., president of the Howard Hughes Medical Institute said: “Obviously, the Institute is quite proud that Jeff’s molecular approach to unraveling the genetics of obesity has been successful. It is gratifying to think that the work may form the basis for new and innovative ways to treat human obesity.”
Phillip Gorden, M.D., director of the National Institute of Diabetes and Digestive and Kidney Diseases, NIH, which helped fund the research, said: “The results at Rockefeller are exciting because we’ve made a major step forward in the search for a human obesity gene. This major breakthrough gives us a new basis for understanding energy regulation and obesity in people.”
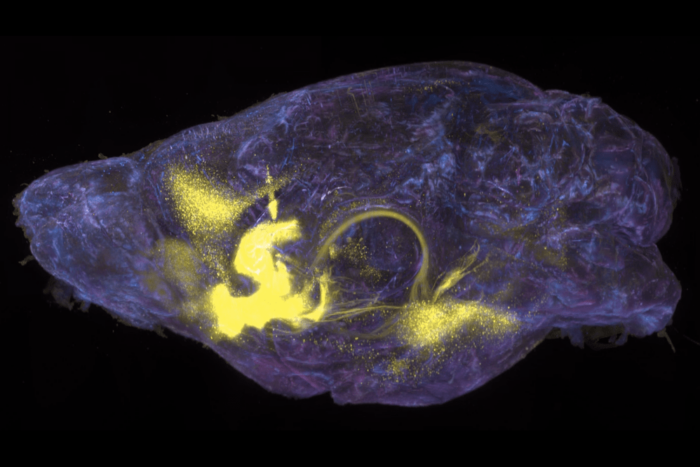
The new findings, which will be reported in the cover story in Nature December 1, show that the mouse gene, ob (for obesity), codes for a protein secreted by adipose tissue. This protein, which contains 167 amino acids, is hypothesized to regulate fat storage by signaling the brain to suppress appetite when the body’s fat stores are sufficient. When mutated in mice, the ob gene no longer delivers its appetite suppressing message and the mice develop a syndrome that resembles extreme obesity and type II diabetes in humans.
“Available data are consistent with the hypothesis that the ob gene product [the protein] functions as part of an endocrine signalling pathway from adipose tissue that signals the hypothalamus–the brain command post for appetite–to regulate the size of the body fat depot,” said Friedman. “This hypothesis now needs to be tested using modern methods of molecular biology.”
Friedman and his colleagues found that the ob gene was completely inactive in one obese strain of mice, an indication that the protein must be made to keep the animal’s weight under control. In a second obese strain, the gene was expressed at 20 times the normal level but contained a mutation that inactivates the protein. The high expression of this mutant is consistent with the idea that the gene encodes a hormone because normally there are feedback loops to shut off hormone production. “Because the gene makes a defective protein in this case,” said Friedman, “the level of hormone production goes up, trying to compensate for its lack of efficacy.” Another indication that the normal protein is a hormone comes from the fact that it contains a “signal sequence” at the amino terminus, a hallmark of proteins secreted from cells, as hormones are.
However, Friedman and his colleague emphasized that it is still necessary to show that the protein does, in fact, function as a hormone that regulates the amount of fat stored in the body. Two crucial experiments will confirm ob’s signalling role: the ob protein must be shown to circulate in the blood, and injections of a normal version of the ob protein must reduce the weight of animals with mutations in their ob genes. Such experiments are now underway in Friedman’s lab.
There is reason to posit that the ob protein is an obesity regulating hormone for humans as well as mice. The physiology of humans and mice is known to be very similar. The Friedman team also found that the protein encoded by the comparable human gene is 84 percent identical to the mouse protein. If the human protein turns out to play a similar role in regulating human obesity as the mouse protein does, then it would be theoretically possible to treat obesity by administering the human protein to patients, much as diabetes is treated with insulin injections. Alternative strategies such as gene therapy (to correct the gene defect) antisense RNA (to intervene in the process of protein production) and pharmaceuticals (to stimulate or block ob’s signalling function) may also prove to be of therapeutic value.
The relevance of this gene to the control of body weight in humans can also be tested by identifying human mutations in ob that contribute to obesity. To this end, Friedman and his Rockefeller colleagues have initiated genetic studies with the residents of the Micronesian Island of Kosrae, where the incidence of obesity is extremely high.
Human obesity, defined as being 20 percent over one’s ideal body weight, is the commonest nutritional disorder in Western societies. Body weight is a highly heritable characteristic, with research showing that anywhere from 60-90 percent of the variability in people’s weights is due to their genes (with enviromental factors such as diet and exercise accounting for the rest). About one in every three Americans suffers from obesity.
Obesity is a major public health problem because it is associated with type II diabetes, hypertension and heart disease. Less well known but equally dangerous are the consequences of being profoundly underweight, a condition that often occurs as a result of serious illnesses such as cancer and AIDS. By revealing the mechanisms that regulate body weight, Friedman’s studies may ultimately lead to ways to boost or diminish the body’s fat stores as appropriate for each individual case.
The Hughes Institute-Rockefeller team’s achievement is the culmination of a long line of research based on the premise that body weight is regulated by a homeostatic feedback system. Combined with observations that an individual’s weight seldom changes dramatically over a lifetime despite a lifetime’s worth of food consumption, scientists hypothesized a feedback system that maintains body weight at a particular “set point.”
In the 1950s and 60s researchers found at least five single genes that lead to obesity in various strains of mice. Two of these genes–ob and db (for diabetes)–appeared to central players in the system, with the ob gene coding for a signalling molecule and the db gene for its receptor. Before that possibility could be tested, scientists had to have the actual genes in hand.
Eight years ago, Friedman and his colleagues began experiments in positional cloning, a technique that allows scientists to snare genes of unknown function. This time-consuming and arduous task was even more difficult in 1986, before the Human Genome Project had generated creative techniques to speed up the process. But the researcher’s pioneering efforts and perseverance paid off in their recent cloning of the ob gene.
“Our success is proof that scientific progress does not happen overnight and that support for basic research is essential,” said Friedman.
Jeffrey M. Friedman, M.D., Ph.D. is an associate investigator with the Howard Hughes Medical Institute and an associate professor and head of the laboratory of molecular genetics at The Rockefeller University. His work was funded in part by NIDDK/NIH. The coauthors of the paper are: Yiying Zhang, Ricardo Proenca, Margherita Maffei, Marisa Barone, and Lori Leopold.