Scientists find evidence that cancer can arise from changes in the proteins that package DNA
A mutation that affects the proteins that package DNA—without changing the DNA itself—can cause a rare form of cancer, according to new findings in this week’s Science from researchers at Rockefeller University.
The mutation is present in histones, the protein scaffolding around which DNA wraps. Researchers have known for some time that histones play a role in switching genes on or off in cells by exposing or covering up various parts of the genome, for instance. But they are just beginning to learn about how changes to these non-DNA structures can affect development and health—a field known as epigenetics—and how they are regulated. Now, for the first time, they’ve shown that a change to the structure of a histone can trigger a tumor on its own.
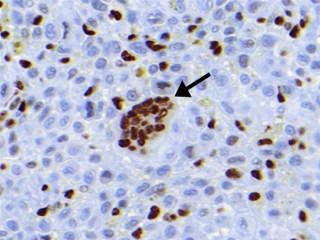
Stuck dividing: In some cancers, including chondroblastoma and a rare form of childhood sarcoma, a mutation in histone H3 reduces global levels of methylation (dark areas) in tumor cells but not in normal cells (arrowhead). Rockefeller scientists found that the mutation arrests the cells in a proliferative state to promote tumor development.
“This is the first study to show that a genetic change to non-DNA structures in the cell—histones—is enough to cause cancer, with no other cooperating DNA mutations,” says co-author Chao Lu, a postdoctoral fellow in the lab of C. David Allis, Tri-Institutional Professor and Joy and Jack Fishman Professor in the Laboratory of Chromatin Biology and Epigenetics at Rockefeller University.
A surprising source
In earlier work, other researchers had found that in approximately 95 percent of samples of chondroblastoma, a benign tumor that arises in cartilage typically during adolescence, carry a mutation in a histone protein called H3.
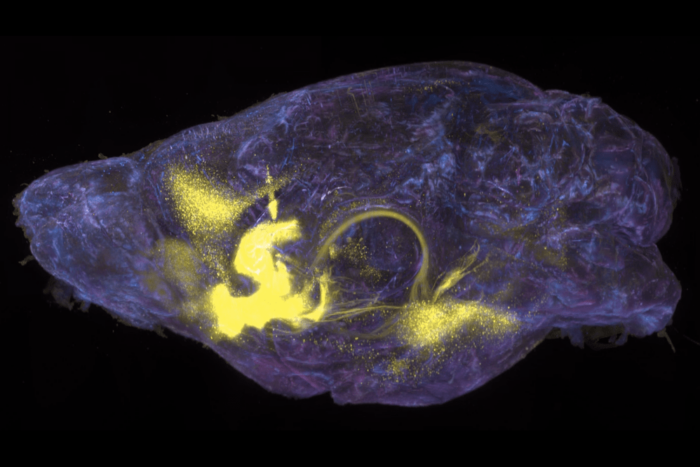
To explore whether and how the mutation causes the tumor, the researchers inserted the H3 histone mutation into mouse mesenchymal progenitor cells (MPCs), which generate cartilage, bone and fat. They then watched these mutant cells lose the ability to differentiate in the lab. Next, they injected the mutant cells into living mice, and the animals developed the tumors rich in MPCs, known as an undifferentiated sarcoma.
“Although researchers knew that a certain type of tumor—chondroblastoma—carried a mutation in the H3 histone and no other mutation, this is the first study to show that the mutation indeed causes tumors, even without any other DNA mutation present,” says Lu.
Next, the researchers tried to understand how the mutation causes the tumors to develop. They found that, when the mutation occurs, the cell becomes locked in a proliferative state—meaning it divides constantly, leading to tumors. Specifically, the mutation inhibits enzymes that normally tag the histone with chemical groups known as methyls, allowing genes to be expressed normally.
In response to this lack of modification, another part of the histone becomes over-modified, or tagged with too many methyl groups. “This leads to an overall resetting of the landscape of chromatin, the complex of DNA and its associated factors, including histones,” says co-author Peter Lewis, a former postdoctoral fellow in the Allis lab and currently an assistant professor at the University of Wisconsin-Madison. This “resetting” is what locks the cell into its proliferative state.
A new target
The findings suggest that researchers should be on the hunt for more mutations in histones that might be driving tumors, says Lu. Meanwhile, he and his colleagues are trying to learn more about how this specific mutation in histone H3 causes tumors to develop. “For instance, we want to know which pathways cause the mesenchymal progenitor cells that carry the mutation to continue to divide, and not differentiate into the bone, fat, and cartilage cells they are destined to become,” he says.
Once researchers understand more about these pathways, says Lewis, they can consider ways of blocking them with drugs, particularly in tumors such as MPC-rich sarcomas—which, unlike chondroblastoma, can be deadly. In fact, drugs that block the pathways may already exist and may even be in use for other types of cancers.
“One long-term goal of our collaborative team is to better understand fundamental mechanisms that drive these processes, with the hope of providing new therapeutic approaches,” says Allis.
This research was supported by The Rockefeller University, a startup provided by the Wisconsin Institute for Discovery, The Greater Milwaukee Foundation, the Starr Cancer Consortium, the Sidney Kimmel Foundation, and the National Institutes of Health (grants P01CA196539, DP2OD007447, R01GM110174, DP2CA174499, K08CA151660, K08CA181475, and P30CA008748).
 Science, online: May 12, 2016 Science, online: May 12, 2016Histone H3K36 mutations promote sarcomagenesis through altered histone methylation landscape Chao Lu, Siddhant U. Jain, Dominik Hoelper, Denise Bechet, Rosalynn C. Molden, Leili Ran, Devan Murphy, Sriram Venneti, Meera Hameed, Bruce R. Pawel, Jay S. Wunder, Brendan C. Dickson, Stefan M. Lundgren, Krupa S. Jani, Nicolas De Jay, Simon Papillon-Cavanagh, Irene L. Andrulis, Sarah L. Sawyer, David Grynspan, Robert E. Turcotte, Javad Nadaf, Somayyeh Fahiminiyah, Tom W. Muir, Jacek Majewski, Craig B. Thompson, Ping Chi, Benjamin A. Garcia, C. David Allis, Nada Jabado, and Peter W. Lewis |